Filmmaker and writer Tahira Kashyap has once again shown remarkable strength and grace in the face of adversity. On World Health Day, she revealed that her breast cancer has relapsed for the second time—seven years after her initial diagnosis in 2018.
In an Instagram post, Tahira candidly shared her experience with her followers. “Seven-year itch or the power of regular screening—it’s a perspective,” she wrote. “I’d like to go with the latter and suggest the same for everyone who needs to get regular mammograms. Round 2 for me… I still got this.”
“When life gives you lemons, make lemonade. When life becomes too generous and throws them again at you, you squeeze them calmly into your favourite kala khatta drink and sip it with all the good intentions. Because, for one, it’s a better drink, and two, you know you will give it your best once again,” she added.
The announcement struck a chord because of her deeply human and relatable message. Many celebrities have shown their support in the comments. Mini Mathur wrote, “You will win round 2 as well Tahira. Stay on course. Keep going.” Guneet Monga said, “I love you! ♥️✨ this too shall pass and come out of this victorious ♥️✨” Husband Ayushmann Khurrana called Tahira, “My hero❤️🥹,” in the comment section.
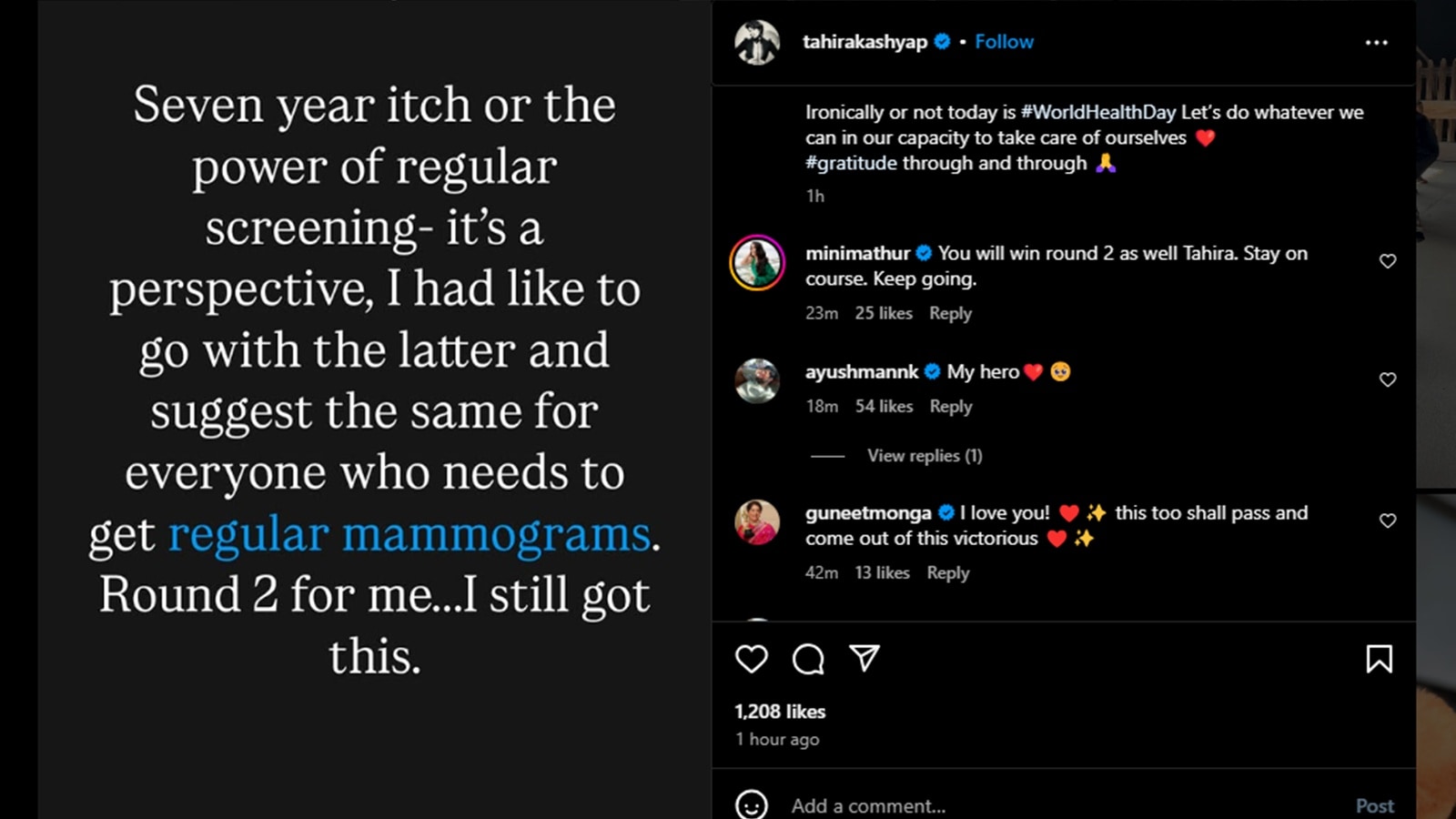 The announcement struck a chord because of how deeply human and relatable Tahira’s message was (Screenshot from Instagram)
The announcement struck a chord because of how deeply human and relatable Tahira’s message was (Screenshot from Instagram)
In her recent post, Tahira reminded everyone of the importance of regular health check-ups and self-awareness. Her words echoed with a call to action—especially for women—to prioritise mammograms and breast cancer screenings.
Dr Tripti Raheja, Lead Consultant – Obstetrics & Gynaecology at the CK Birla Hospital, Delhi, says having cancer once can make a person more susceptible to recurrence. There are several reasons why this happens.
Even after successful treatment—such as surgery, chemotherapy, or radiation—some microscopic cancer cells may remain undetected in the body. Over time, these cells can grow again and lead to a recurrence, Dr Raheja said.
“The risk of cancer coming back also depends on the type and stage of the original cancer. For example, some cancers, like triple-negative breast cancer, are more aggressive and more likely to return, particularly within the first few years after treatment,” she explained.
Story continues below this ad
Genetic and biological factors also play a role; individuals with inherited mutations, such as BRCA1 or BRCA2, are at higher risk of recurrence or developing new cancers. Additionally, lifestyle habits such as smoking, alcohol use, obesity, and chronic inflammation, along with hormonal imbalances, can increase the likelihood of cancer returning—especially in hormone-sensitive cancers.
According to Raheja, as we age or if the immune system is compromised, the body’s ability to fight off abnormal cell growth also weakens, contributing to the risk. So yes, while treatment may be effective, the nature of cancer and various risk factors can make some individuals more vulnerable to it coming back.
Why are regular screenings important? How often to get them
Regular screenings and mammograms are critical for early detection and are especially important for women who have had breast cancer in the past, Dr Raheja said. “These individuals face a higher risk of recurrence in the same breast or chest wall, or of developing a new cancer in the opposite breast.”
After undergoing breast-conserving surgery like a lumpectomy, most women are advised to have a mammogram once a year. In some cases, especially if the previous cancer was aggressive or if the patient is younger, doctors may recommend screening every six months for the first two to three years.
Story continues below this ad
For women who have had a unilateral mastectomy, annual mammograms are typically advised for the remaining breast. In the case of bilateral mastectomy (removal of both breasts), routine mammograms may no longer be necessary, though regular clinical exams and body awareness remain essential.
Based on individual risk factors, additional imaging like breast ultrasound or MRI may also be recommended, particularly for younger women or those with dense breast tissue. Ongoing follow-up care should always be tailored to the individual, in close consultation with their healthcare provider.
DISCLAIMER: This article is based on information from the public domain and/or the experts we spoke to. Always consult your health practitioner before starting any routine.


